The link between eczema and depression
Eczema is a chronic condition that causes patches of dry, itchy, and inflamed skin. It has links to conditions such as asthma, food allergies, and skin infections.
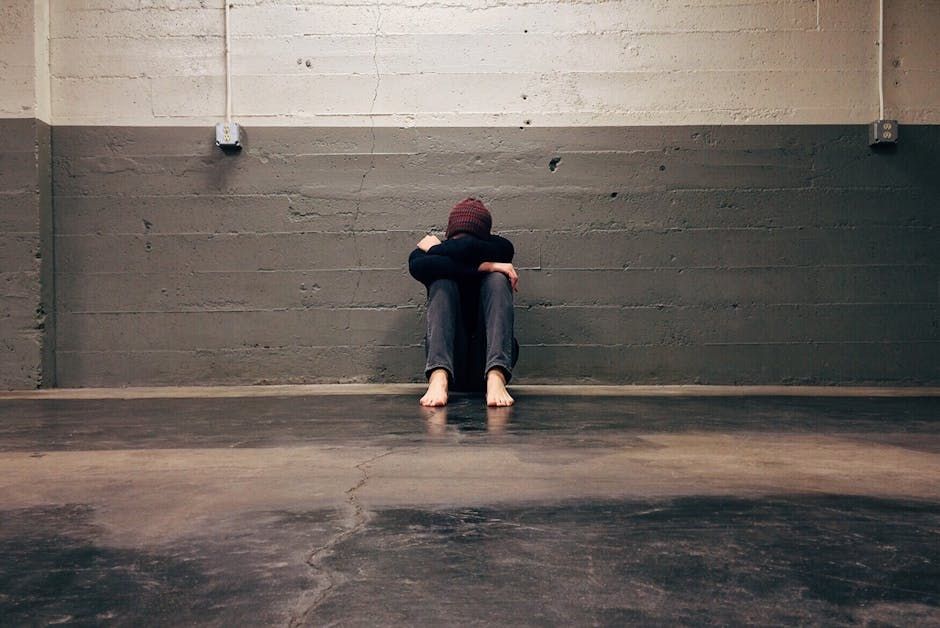
Eczema also has links with mental health conditions such as stress, anxiety, and depression. Mental health conditions may trigger an eczema outbreak.
At the same time, an eczema flare-up may cause a person to feel more stressed, anxious, or depressed. They may also experience fatigue and social withdrawal due to their physical and mental health symptoms.
However, there are several ways to treat eczema and mental health conditions.
This article explores the connection between eczema and depression. It also looks at the potential treatment options and the support available for mental health.
What is eczema?
Eczema is an autoimmune condition, which occurs when a person has an overactive immune system. This creates an inflammatory effect in the body, harming the skin barrier and increasing susceptibility to bacteria, allergens, and irritants.
Eczema causes skin irritation, itchiness, and swelling. Additional symptoms of eczema include bumps, discolored rashes, and scaly skin.
Of the seven types of eczema, atopic dermatitis is the most common. It is the type most likely associated with related health conditions, including mental health conditions such as anxiety and depression.
Atopic dermatitis often occurs in people who also have asthma , food allergies , and hay fever. The link between eczema and mental health In addition to causing physical symptoms, eczema can affect a person’s mental and emotional well-being.
In fact, researchers have linked eczema with several mental health conditions, including stress, anxiety, and depression. Although the exact reasons are unclear, there are several potential causes of these connections.
Research from 2019 indicates that depression is more common in people with autoimmune conditions such as atopic dermatitis. The study authors suggest that this may be due to inflammatory changes in the brain relating to anxiety and depression.
According to some other 2019 research, people with atopic dermatitis are significantly more likely to experience suicidal ideation and suicide attempts. The researchers suggest that this may partially be due to the effects of atopic dermatitis.
The condition can cause debilitating skin symptoms, sleep loss, and psychosocial factors such as stigmatization, shame, and impaired school or work performance. Often, eczema and mental health conditions feed off each other, with eczema symptoms negatively affecting mental health and vice versa.
Stressful emotions or events may trigger the fight-or-flight response, thereby elevating stress hormones such as adrenaline and cortisol. Research from 2020 suggests a relationship between developing depression and the severity of atopic eczema.
Having high cortisol levels can increase skin inflammation and oil production in the skin glands, leading to clogged pores and breakouts. This can also cause a flare-up or worsen existing eczema symptoms.
Elevated cortisol levels may also weaken the immune system, making it harder for the body to fight skin infections and regenerate skin to promote healing. Help is out there If you or someone you know is in crisis and considering suicide or self-harm, please seek support: Call or text the 988 Lifeline at 988 or chat at 988lifeline.org.
Caring counselors are available to listen and provide free and confidential support 24/7. Text HOME to the Crisis Text Line at 741741 to connect with a volunteer crisis counselor for free and confidential support 24/7.
Not in the United States? Find a helpline in your country with Befrienders Worldwide.
Call 911 or your local emergency services number if you feel safe to do so. If you’re calling on behalf of someone else, stay with them until help arrives.
You may remove weapons or substances that can cause harm if you can do so safely. If you’re not in the same household, stay on the phone with them until help arrives.
Depression and eczema Mental health conditions such as stress, anxiety, and depression may cause an eczema flare-up or worsen existing symptoms. This can cause a person to feel more stressed, anxious, or depressed.
Those with depression and eczema may feel embarrassed, ashamed, or hopeless about their situation, which can affect their mental well-being. They may also withdraw from or avoid social activities, relationships, or physical activities, which can worsen symptoms of depression.
Eczema and depression are associated with sleep disturbances. The discomfort and itchiness relating to eczema may interfere with sleep, and people with depression may find it more difficult to fall asleep, sleep deeply, and get enough sleep.
A lack of quality sleep may cause irritability, moodiness, and depression.
It can also affect concentration, motivation, and emotion regulation.
Treatment
options
Treatment
options for depression and eczema involve conventional methods, complementary therapies, and natural remedies.
A person can work with a healthcare professional to create an individual treatment plan that best fits their needs.
Treatment
for eczema involves healing irritated skin
, reducing the severity of the symptoms, and preventing future outbreaks. It is also important to identify and avoid triggers.
Some eczema treatment options include: applying aloe vera , coconut oil , or apple cider vinegar to the skin trying wet wrap therapy taking a baking soda, colloidal oatmeal, or Epsom salt bath trying phototherapy using UVA or UVB waves receiving biologic drug injections using prescription topical corticosteroid creams and ointments taking corticosteroids or immunosuppressants using a humidifier bathing and moisturizing daily switching to an anti-inflammatory diet Learning to relax mentally and physically may also help relieve stress, decrease inflammation, and ease symptoms of eczema and depression.
Practicing relaxation techniques may also improve how a person handles and reacts to stressful situations, including eczema flare-ups. Some ways to manage and relieve stress include: meditation mindfulness massage therapy breathing techniques visualization music therapy hypnosis biofeedback tai chi yoga yoga nidra exercise sleep trying creative activities doing enjoyable activities spending time with loved ones spending time in nature trying a digital detox Mental health support Psychotherapy, or talk therapy, is a popular and effective treatmentfor depression.
The most common types are cognitive behavioral therapy (CBT) and interpersonal therapy. Psychotherapy teaches people to improve their thought patterns, behaviors, and emotional issues.
This can positively affect their relationships, communication, and social functioning. To ease the symptoms and severity of depression, people can also take oral medications such as: antidepressants, including: selective serotonin reuptake inhibitors (SSRIs) serotonin-norepinephrine reuptake inhibitors (SNRIs) bupropion antianxiety medications, including benzodiazepines mood stabilizers, including lithium antipsychotic medications
Summary
Eczema is a chronic inflammatory skin condition that causes patches of dry, irritated, and itchy skin.
The most common type, atopic dermatitis, has links to several mental health conditions, including depression.
Understanding the relationship between eczema and depression
can help a person manage their symptoms and make positive changes. A healthcare professional or mental health specialist can recommend an appropriate eczema and depression treatment plan that combines conventional methods, alternative healing techniques, and positive lifestyle changes.
This can help ease physical symptoms, boost mental health, and improve overall well-being.




